|
October 10, 2009, Is World Mental Health Day
by Christina J. Ansted, MPH
On Saturday, October 10, 2009, the World Federation for Mental Health (WFMH) celebrates World Mental Health Day. The mission of the WFMH is “Making Mental Health a Global Priority”, and they’ve been doing just that for more than 61 years. Having celebrated their 60th anniversary in 2008, the resolution to found WFMH began with a meeting in the British Ministry of Health building during the London Congress on the night of August 18 and completed on the night of August 19, 1948.(1) Although the world we live in is a very different place today than it was more than half a century ago, many stigmas surrounding mental illness still persist in society, both in the public domain and behind closed doors. This year, the WFMH approaches World Mental Health Day by looking at mental health in primary care—enhancing treatment and promoting mental health. World Mental Health Day 2009 will highlight the opportunities and challenges that integrating mental health services into the primary healthcare delivery system will present, not only to people living with poor mental health, their families, and caregivers, but also to healthcare professionals and providers.(2)
It should come as no surprise that most individuals go to their primary care doctor as a first line of defense against illness, be it physiological or mental. Those patients who are thought to have a mental illness or psychiatric need are typically referred to a psychiatrist for appropriate diagnosis and treatment. Then there are those patients who enter the healthcare system by way of the emergency room. These are the patients who may present during a psychotic episode or who are brought to a hospital by family, friends, or even sometimes law enforcement. And for these patients, optimal communication with their primary care physician can be difficult or impossible. Many do not know who their primary care physician is, and many more still are without a support system that can help fill in the blanks.
What becomes apparent is that physical health and mental health are seen as two separate entities. One physician takes care of the brain and the other the body. Psychiatrists are trained to heal the brain and its collection of conscious and unconscious cognitive processes known as “the mind.” Primary care is supposed to heal the body and refer to a specialist as needed when specific expertise is required. Today it is more important for all clinicians to think of the overall health and well-being of each patient, which includes both physical and mental health.
For patients with severe mental illness such as schizophrenia, their mental illness can easily become the focus of care, not their obesity, hypertension, or diabetes. Persons diagnosed with schizophrenia have higher morbidity and mortality rates from cardiovascular disease, and yet they often have limited access to appropriate screening or treatment. Metabolic disorders are highly prevalent in patients with schizophrenia, exceeding 50% in some studies.(3) In a 2008 survey conducted by Mental Health America (MHA), 74% of responding psychiatrists felt that they were not as well-equipped to address the patient’s overall health as are primary care physicians.(4) The primary care physician can be an integral agent of change in the mental health of patients. The primary care physician has the possibility of more continuous and permanent contact with the patient.(5) In reality, primary care and psychiatry overlap more than they differ, which would suggest a need to bridge the gap between the two disciplines. It could further be argued that more than being two separate parts, primary care and psychiatry represent a bifurcation of the common whole—one branch cannot exist in a vacuum without the other. In other words, they are inextricably linked.
The linking of healthcare services, or “integration”, has become a focal point of optimizing care. To aid in the integration of mental health efforts, the World Health Organization (WHO) and the World Organization of Family Doctors (Wonca) have come together to identify 10 principles for integration. These principles cover everything from policy and training to human resources and collaborative care. Across the full spectrum of political and economic contexts, and levels of the health system, these 10 principles are “non-negotiable” for integrated primary mental healthcare.(6)
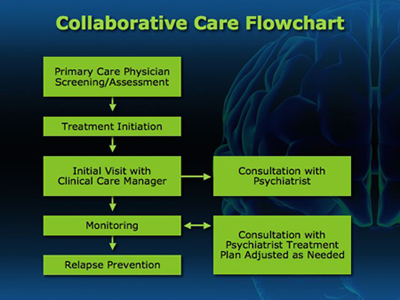
The idea of collaborative care is not a new one per se, but the concept has been gaining ground in recent years as essential for improving the care of mental health patients. To that end, the Hogg Foundation out of Austin, Texas, provides us with an interesting pictorial of the ideal flow for collaborative care between psychiatry and primary care (see figure below).(7)
The importance of integration between psychiatry and primary care cannot be overlooked in the optimization of care for patients with mental health disorders, and reaching a point of optimal care requires not only crossing the chasm of improved communication within the healthcare system, but also complex and unpredictable combinations of psychosocial interventions and social support systems. Mental health affects us all. On October 10, take a moment to remember those affected by mental health disorders, and think about what each of us can do to help improve their lives.
Do you have feedback for the author? Click here to send us an email.
Download printable version here.
References
- World Federation for Mental Health. A Brief History. Available at http://www.wfmh.org/03Briefhistory.htm. Accessed on October 2, 2009.
- World Federation for Mental Health. Mental Health in Primary Care: Enhancing Treatment and Promoting Mental Health [PDF]. 2009. Available at http://www.wfmh.org/00WorldMentalHealthDay.htm. Accessed on October 2, 2009.
- Nasrallah H, et al. Low rates of treatment for hypertension, dyslipidemia and diabetes in schizophrenia: data from the CATIE schizophrenia trial sample at baseline. Schizophr Res 2006;86(1-3):15-22.
- Mental Health America. Mental Health and Psychiatry News. 2008. Available at http://www.health.am/psy/more/schizophrenia-and-healthcare-survey. Accessed on October 1, 2009.
- Fahrer R. Psychiatric training of the primary care physician in the general hospital. Mental Health in Primary Care: Enhancing Treatment and Promoting Mental Health [PDF]. 2009;24-25. Available at http://www.wfmh.org/00WorldMentalHealthDay.htm. Accessed on October 2, 2009.
- WHO/Wonca. Integrating Mental Health into Primary Care – A Global Perspective. 2008;49-55. Available at http://www.globalfamilydoctor.com/PDFs/
IntegratingMentalHealthIntoPrimaryCare.pdf?nav_id=339
- Hogg Foundation for Mental Health - Integrated Health Care. Mental Health in Primary Care: Enhancing Treatment and Promoting Mental Health [PDF]. 2009;17-18. Available at http://www.wfmh.org/00WorldMentalHealthDay.htm. Accessed on October 2, 2009.
|
|